How Healthcare Vulnerabilities Exacerbated the COVID Pandemic in Mexico
- Pre-Collegiate Global Health Review

- Apr 27, 2023
- 8 min read
Austin Roberts, Saline High School, Saline, Michigan, USA

For the past three years, COVID-19 has impacted lives across the globe. The World Health Organization (WHO) estimates that 622 million people globally have been infected with the coronavirus at some point during the pandemic. Of those, over 6.5 million have lost their lives to the virus (World Health Organization, 2022). For countries that were unprepared, COVID-19 overwhelmed their healthcare systems and caused hospitals to overflow as they ran out of beds. Among these, Mexico provides an example of a healthcare system that was ill-equipped and underprepared to face the mountain of hospitalizations that confronted it in 2020. Lack of healthcare coverage, poor quality care, and substandard government response caused an already at-risk population to contract more than 7 million cases of the coronavirus.
The first of many problems with the Mexican healthcare system is poor insurance coverage, which led to many preventable deaths not just during, but before the coronavirus pandemic. Depending on employment status, Mexican citizens receive universal health insurance provided to them by their government. Private sector employees are covered by the IMSS (Instituto Mexicano de Seguro Social), and public sector employees are covered by the ISSSTE (Instituto para la Seguridad y Servicios Sociales para las Trabajadores del Estado). There are also other, much smaller programs for more specific employees, such as those who work for PEMEX (Petroleo Mexicano), the government-owned petroleum company. Citizens who do not qualify for coverage under any employment-based system received nearly free healthcare coverage under a program called Seguro Popular until January 2021, when, due to issues with corruption and lack of universality, it was replaced by a modern program called the INSABI (Instituto de Salud para el Bienestar) (Huendo, 2021). The fragmented nature of Mexico’s health coverage does not allow for portability, which means that patients covered by one organization cannot receive services from another, even if one system has a shortage of patients and the other has a surplus. A patient covered by ISSSTE who wants to pick up a prescription has to go to an ISSSTE pharmacy to pick up their prescription, even if the only pharmacy around is an IMSS facility. This forces them to either drive long-distances or to pay out-of-pocket at a retail pharmacy (Mexican Healthcare System, 2015). The added difficulty in accessing treatment led citizens to avoid seeking services they needed because they were too difficult to obtain. Lack of widespread access to health insurance forced many Mexican citizens to choose between paying for lifesaving treatment for their family members and being able to pay for basic living expenses. Additionally, while Seguro Popular was widely viewed as a step forward in providing universal healthcare coverage to all Mexican citizens, it still suffered from lack of universality, as nearly 20 million people never enrolled (Browner and Fernandez, 2022). Even those that participated were not provided much support because Seguro Popular relied heavily on out-of-pocket spending, and healthcare expenses pushing low-income citizens deeper into poverty were common (Mexican Healthcare System, 2015).
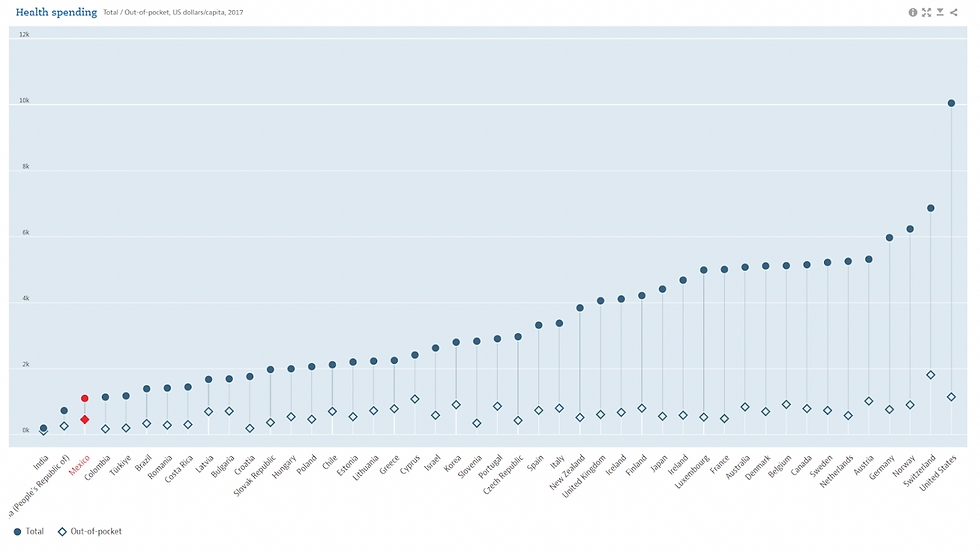
Figure 1: This Organization for Economic Cooperation and Development (OECD) graph compares the total spending on healthcare by citizens, insurance, and the government with the out-of-pocket costs paid by patients of 45 countries in 2015. Mexico, (highlighted in red) had nearly 40% of healthcare expenditures come out of the pockets of its citizens. Compared to the US (far right), with only around 10% out of pocket costs, Mexico’s Seguro Popular was not as effective as other countries’ social welfare programs (OECD Health Spending, 2022).
Corruption was a major problem for the Seguro Popular program as well. Between 2010 and 2019, approximately 178 million USD of government funding intended for public healthcare mysteriously disappeared before hospitals received them. While the final destination of these funds is unknown, it is speculated that the money was spent by public officials for personal use (Gonzalez-Aquines, 2020). The number of lives that could have been saved with 178 million USD of extra funding is impossible to know for sure, but it’s likely that it could have prevented thousands of extra deaths.
In addition to inadequate insurance benefits for its citizens, an underfunded healthcare system has been another major problem facing the Mexican government. In 2019, the Mexican government spent 2.8% of its GDP on the domestic government health system, which is less than half the 6% spending recommended to countries by the Pan American Global Health Organization (Huendo, 2021). In terms of total healthcare spending, Mexico spent roughly 6.2% of their GDP in 2015. This is one of the lowest rates in the OECD and well below the OECD average of 9.6% (Mexican Healthcare System, 2015). This lack of funding corresponds to a lack of safety and quality. In 2019 alone, there were 17,358 reports of medical negligence to Mexico’s national commission for medical arbitration. This is thought to be an underestimation due to under-reporting and patients’ lack of knowledge about their rights (Huendo, 2021). The reputation for poor-quality care has led Mexicans to avoid going to the hospital and in some cases even waiting until their conditions have progressed to the point where doctors can do very little to help them (Oré, 2021).
Another factor that increases strain on the already struggling health system is the prevalence of risk factors in the Mexican population. Childhood obesity, caused and compounded by a lack of healthy eating options in schools, a sedentary lifestyle, and public lack of understanding about general health, continues to be a public health obstacle for Mexico’s government (Aceves-Martins et al., 2016). This problem has continued into adulthood as well: in the 2017 OECD obesity update, Mexico had an obesity rate of 32.4% (OECD, 2017). Class 2 and 3 obesity has been linked to significantly higher risk of all cause mortality when compared to the normal weight range (Flegal et al., 2013). This left the obese population more vulnerable to severe COVID complications. Another factor contributing to drastically increased risk of all cause death is smoking. A 2021 study found that daily smoking contributes to all-cause mortality and is strongly associated with diseases such as Chronic Obstructive Pulmonary Disease (COPD) (Thompson et al., 2021). COPD is particularly troublesome, as it impacts the lungs and has been linked to increased risk of severe illness and hospitalization when infected with the coronavirus (Leung et al., 2020). These societal vulnerabilities increased the burden on hospitals when the pandemic finally struck.
At the onset of the coronavirus in Mexico, President Andrés Manuel López Obrador (AMLO) was skeptical of the gravity of the pandemic, and questioned scientific consensus on containment of the virus. His resistance to public safety measures such as social distancing and mask mandates effectively placed the burden of controlling the coronavirus on the shoulders of state lawmakers (Bennouna et al., 2021). The lack of coordination in state response led to variation in national policy, where some states did not implement enough restrictions to properly contain the virus (Knaul et al., 2021). At the national level, Mexico was transitioning from the now-defunct Seguro Popular to the more modern INSABI institution. In order to accomplish his goal of reducing corruption, Obrador reduced services provided by the private sector in his public healthcare plan. This included distribution companies, which led to widespread supply issues. In October 2021, INSABI had only delivered 9.5% of the drugs requested by states since it took effect in January, meaning that even people without COVID-19 were lacking in access to lifesaving medication (Bello, 2021). The lack of healthcare resources didn’t just stop at prescription medication, however. In 2021, a shortage of portable oxygen tanks ravaged Mexico City, affecting the impoverished the most. With nearly 90% of the city’s COVID beds full, demand outpaced supply, and the cost to refill a 24-hour portable oxygen tank rose to around $160, more than 20 times the minimum daily wage of 7 USD. As prices shot up, people with respiratory disorders or severe complications from the coronavirus itself began to suffocate with empty oxygen tanks and no way to refill them. Eventually, a city-based program that allowed residents to refill their tanks for free was established in Iztapalapa and Gustavo Madero, but the shortage wasn’t exclusive to Mexico City. Elsewhere, the problem only worsened as people became so desperate that they robbed hospitals at gunpoint for oxygen to save their own lives (Oré, 2021).
Medical supply shortage was not the only aspect that led to preventable deaths. Medical negligence and malpractice also led Mexicans to fear going to the hospital. Doctors working in hospitals treating ISSSTE beneficiaries reported that, on top of poor sanitation practices, patients who tested positive for the coronavirus were being mixed with non-infected patients with little regard for cross-contamination. Unsurprisingly, the hospital became a hotbed for COVID-19 cases (Rondero, 2020). Mexican hospitals’ reputation of malpractice led the general Mexican to fear visiting the hospital. In fact, a survey by El Financiero found that 40% of respondents felt very unsafe sending a loved one to the hospital (Moreno, 2020). Avoiding doctor’s offices and public hospitals led to thousands dying before seeking treatment (Kitroeff and Villegas, 2020). Among those who did seek care, many found that hospitals were too full to treat them. In early November 2020, just eight months after the start of the pandemic, El Universal reported that at least 94 out of Mexico’s 949 COVID hospitals reported being at full capacity.

Figure 2: This OECD indicator displays the number of total hospital beds per 1000 citizens for every OECD country. Based on the latest data available, Mexico (labeled blue) had the lowest number of hospital beds per 1000 people in the entire OECD at only 1.0 beds per 1000 citizens (OECD Hospital Beds Indicator, 2022).
In the present, Mexico’s government has begun to relax what little coronavirus restrictions it implemented during the more intense days of the pandemic. The few partial shutdowns of businesses have been lifted and Mexico’s government has announced a shift from a pandemic to an endemic policy, as around 90% of the population has received at least one dose of the COVID vaccine (Medical Press, 2022). The future of Mexican healthcare is uncertain, but there has been speculation that the coronavirus pandemic will spur greater cooperation between the United States and Mexico in order to prevent the spread of future pandemics (Rudman and Wood 2020). International cooperation has been proven to be an important component in vaccine distribution, streamlined creation of international regulatory bodies, and improving global health sovereignty (Fattibene, 2022). Studying health from a global perspective means examining more than just one country's part in global health. It requires broadening one’s view beyond that of a single country and looking at the issues encountered around the world. The challenges detailed in this paper are not exclusive to just Mexican healthcare; in Africa, barriers such as poverty and restrictive social norms lead patients to avoid seeking treatment for their medical problems. The importation of essential healthcare resources is necessary to supplement a struggling manufacturing sector, and this raises the cost of treatment for an already-impoverished population to the point that people cannot afford to seek the care they need. Additionally, societal expectations for women to only seek medical care with a man’s permission and a stigma around unwed women receiving maternal and reproductive care leads women not to seek treatment for their conditions, resulting in preventable deaths across the continent (Executive Summary, 2021). Similarly, healthcare corruption, particularly problematic in second and third-world countries, affects more than just Mexico. In Uganda, for example, a study found that doctors were paid so little that their main source of income came from the illegal resale of pharmaceuticals (Bouchard et al., 2012). Furthermore, a variety of forms of corruption exist in Anglophone West Africa, including paying bribes for employment, forgery of documents, and workers being hired based on relationships with people with political connections (Onwujekwe et al., 2019). With new diseases evolving every day, examining our failures and flaws as a planet is vital to preventing future loss of life.
References
Aceves-Martins M, Llauradó E, Tarro L, Solà R, Giralt M. Obesity-promoting factors in Mexican children and adolescents: challenges and opportunities. Glob Health Action. 2016 Jan 18;9:29625. doi: 10.3402/gha.v9.29625. PMID: 26787421; PMCID: PMC4718931.
Bello M. 2021 Oct 8. INSABI Medicine Supply for 2021 at Less Than 10 Percent. Mexico Business. [accessed 2022 Oct 12]. https://mexicobusiness.news/health/news/insabi-medicine-supply-2021-less-10-percent.
Bennouna C, Giraudy A, Moncada E, Rios E, Snyder R, Testa P. Pandemic Policymaking in Presidential Federations: Explaining Subnational Responses to Covid-19 in Brazil, Mexico, and the United States. Publius. 2021 Aug 14:pjab025. doi: 10.1093/publius/pjab025. PMCID: PMC8385998.
Bouchard M, Kohler JC, Orbinski J, Howard A. 2012. Corruption in the health care sector: A barrier to access of orthopaedic care and medical devices in Uganda. BMC International Health and Human Rights. 12(1). doi:10.1186/1472-698x-12-5. [accessed 2019 Oct 19]. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3492067/.
Browner CH, Fernández GL. 2022 Jun 8. The Mexican Health Care System Under the Administration of AMLO. NACLA. [accessed 2022 Oct 3]. https://nacla.org/mexican-health-care-system-under-administration-amlo.
Executive Summary: The State of Universal Health Coverage in Africa. Africa Health Agenda International Conference (AHAIC). https://ahaic.org/download/executive-summary-the-state-of-universal-health-coverage-in-africa/.
Fattibene D. 2022 May 9. Global Health and International Cooperation. IAI Istituto Affari Internazionali. [accessed 2022 Dec 1]. https://www.iai.it/en/pubblicazioni/global-health-and-international-cooperation.
Flegal KM, Kit BK, Orpana H, Graubard BI. 2013. Association of All-Cause Mortality With Overweight and Obesity Using Standard Body Mass Index Categories. JAMA. 309(1):71. doi:10.1001/jama.2012.113905.
Gonzalez-Aquines A. 2020 Oct 30. Health corruption: a chronic-degenerative illness in the public health sector. 2020 Oct 30. Eye on Global Health. https://eyeonglobalhealth.com/2020/10/30/health-corruption-a-chronic-degenerative-illness-in-the-public-health-sector/.
Huendo A. 2021 Jan 21. Killer Hospitals and COVID-19 in Mexico – La Gente Newsmagazine – University of California, Los Angeles. [accessed 2022 Sept 29]. https://lagente.org/killer-hospitals-and-covid-19-in-mexico/.
Kitroeff N, Villegas P. 2020 Aug 10. “I’d Rather Stay Home and Die.” The New York Times. [accessed 2022 Sept 29]. https://www.nytimes.com/2020/08/10/world/americas/mexico-coronavirus-hospitals.html
Knaul F, Arreola-Ornelas H, Porteny T, Touchton M, Sánchez-Talanquer M, Méndez Ó, Chertorivski S, Ortega S, Chudnovsky M, Kuri P; group from the Observatory for the Containment of COVID-19 in the Americas. Not far enough: Public health policies to combat COVID-19 in Mexico's states. PLoS One. 2021 Jun 1;16(6):e0251722. doi: 10.1371/journal.pone.0251722. PMID: 34061864; PMCID: PMC8168889.
Leung JM, Niikura M, Yang CWT, Sin DD. COVID-19 and COPD. Eur Respir J. 2020 Aug 13;56(2):2002108. doi: 10.1183/13993003.02108-2020. PMID: 32817205; PMCID: PMC7424116.
Mexican Healthcare System Challenges and Opportunities. 2015. https://www.manatt.com/uploadedFiles/Content/5_Insights/White_Papers/Mexican%20Healthcare%20System%20Challenges%20and%20Opportunities.pdf.
Mexico says coronavirus now endemic, not pandemic. medicalxpresscom. [accessed 2022 Nov 1]. https://medicalxpress.com/news/2022-04-mexico-coronavirus-endemic-pandemic.html.
Moreno A. 2020 Jul 30. 86% de los mexicanos sí cree en la utilidad de los cubrebocas para prevenir el COVID-19. El Financiero. [accessed 2022 Oct 28]. https://www.elfinanciero.com.mx/nacional/86-de-los-mexicanos-si-cree-en-la-utilidad-de-los-cubrebocas-para-prevenir-el-coronavirus/.
Onwujekwe O, Agwu P, Orjiakor C, McKee M, Hutchinson E, Mbachu C, Odii A, Ogbozor P, Obi U, Ichoku H, et al. 2019. Corruption in Anglophone West Africa health systems: a systematic review of its different variants and the factors that sustain them. Health Policy and Planning. 34(7):529–543. doi:10.1093/heapol/czz070.
OECD (2022), Health spending (indicator). doi: 10.1787/8643de7e-en (Accessed on 20 October 2022)
OECD (2022), Hospital beds (indicator). doi: 10.1787/0191328e-en (Accessed on 02 November 2022)
Oré D. 2021 Jan 21. Runaway cost of oxygen tanks adds extra agony to pandemic in Mexico. 2021 Jan 21. Reuters. [accessed 2022 Sept 30]. https://www.reuters.com/article/us-health-coronavirus-mexico-oxygen-idUKKBN29Q2NG.
Rondero L. 2020 Sep 11. Denuncian grave negligencia médica por Covid-19 en ISSSTE. MetrópoliMx. [accessed 2022 Sept 29]. https://metropolimx.com/denuncian-grave-negligencia-medica-por-covid-19-en-issste/.
Rudman AI, Wood D. 2020. Pandemics and Beyond: The Potential for U.S.-Mexico Cooperation in Public Health. [accessed 2022 Oct 28]. https://www.wilsoncenter.org/sites/default/files/media/uploads/documents/Beyond%20Pandemics.pdf
Thomson B, Tapia-Conyer R, Lacey B, Lewington S, Ramirez-Reyes R, Aguilar-Ramirez D, Gnatiuc L, Herrington WG, Torres J, Trichia E, et al. 2021. Low-intensity daily smoking and cause-specific mortality in Mexico: prospective study of 150 000 adults. International Journal of Epidemiology. 50(3):955–964. doi:10.1093/ije/dyab013.
World Health Organization. 2022. WHO COVID-19 dashboard. World Health Organization. https://covid19.who.int/.




I'm Jefferey Vargas. My girlfriend ended our relationship for seemingly no reason and I came to understand that my financial struggles may have contributed to this, as a healthy relationship is difficult without money and aside from God, having more money is often seen as vital. For spell expertise, Lord Meduza is the right person to turn to. My girlfriend left me for another man due to my financial situation but after connecting with Lord Meduza he created a spell that not only brought my girlfriend back but also made me a lottery winner of €116 million by providing me with the 6 lucky numbers to play the lottery. Everything feels almost unreal but I assure you this is genuine…